This is a continued from my prior blog post titled, “Emergency Room Standard of Care; Failure to Diagnose and Delay in the Treatment of a Head Injury ~ part one,” with some more of the questions that should be asked and answered in a Medical Malpractice Case in evaluating whether or not the Standard of Care was breached in the Failure to Diagnose and Delay in the Treatment of a Head Injury in the ER:
3.) Q: What Injuries Did the Patient Sustain?
Why is this important? Patients who sustain severe and complicated trauma injuries may need to be transported to a certified trauma center. Therefore, it is imperative that the severity of the Patient’s injuries be determined as early as possible.
4.) Q: Was the Patient Intubated?
Why is this important? As described above, intubation and ventilation is required in patients with a low GCS score.
5.) Q: Did the Patient have Any Comorbidities?
Why is this important? Anti-coagulation use may increase the risk for intra-cranial hemorrhage following a head injury so it is very important to know whether or not the patient had any comorbidities.
6.) Q: Was Oxygen Administered?
Why is this important? Once the patient’s airway has been secured, then he or she must be maintained on adequate oxygenation level, starting at 100%.
7.) Q: Did the EMS Personnel Transport the Patient to a Trauma Center?
Why is this important? As stated herein above, once the severity of the patient’s injuries are determined, then if the patient is suspected to have a head injury the patients should to be transported to the trauma center as soon as possible.
8.) Q: Was the Patient’s Spine Immobilized?
Why is this important? It is imperative that the patient’s cervical spine is immobilized to prevent further injury.
9.) Q: With what Symptoms did the Patient Present?
Why is this important? If the patient presented with these, or similar, symptoms, then a head injury may likely be suspected: 1.) Symptoms of increased ICP include vomiting, syncope, altered mentation, bradycardia; 2.) Increased blood pressure; and 3.) Irregular respirations.
10.) Q: Were the Patient’s Vital Signs Monitored During Transportation?
Why is this important? En-route to the hospital or nearest trauma center, a three-lead electrocardiogram, pulse oximetry and blood pressure monitoring, must be continuously performed during transportation.
11.) Q: What was the Patient’s Glasgow Coma Score upon Admission?
Why is this important? As stated previously, the standard internationally accepted measurement of consciousness is the Glasgow Coma Scale, and the scale ranges from 0-15. The lower the number on the scale, then the more severe the head injury.
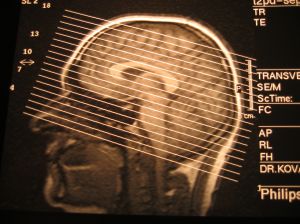
12.) Q: Did the ER physician order a CT scan of the patient’s head?
Why is this important? A CAT Scan is the procedure of choice for emergent assessment of brain/head injury since the CAT Scan is rapid, readily available and reliably shows acute hemorrhages and skull fractures.
13.) Q: Was the CT Scan Suggestive of a Trauma to the Brain?
Why is this important? If the imaging studies from the CT Scan are suggestive of brain trauma, then a neurological referral is needed as soon as possible.
I will continue this discussion in my next blog post titled, “Emergency Room Standard of Care; Failure to Diagnose and Delay in the Treatment of a Head Injury ~ part three,” with some final questions that should be asked and answered in a Medical Malpractice Case in evaluating whether or not the Standard of Care was breached in the Failure to Diagnose and Delay in the Treatment of a Head Injury in the ER.
At Julie A. Rice, Attorney at Law, & Affiliates, we are experts in Medical Malpractice cases whether or not said cases involve the ER so please Contact Us for your free legal consultation if you suspect that you or a loved one has been injured or killed due to the negligence of a healthcare provider whether or not it was in the ER or otherwise. We are here to assist you and we look forward to hearing from you soon.